I was emboldened, upon arriving at the Mayo Clinic ‘s Centre for Innovation last week, to learn that people with deep domain knowledge do not make the best innovators. I concluded that I was therefore well-qualified to warn one of the top academic medical centres in the world, each of whose 60,000 staff knows more about medicine than I do, about the risk of catabolic collapse in the US health system – and what to do about it.
[The 20 minute video of my talk is here.This text touches on: ‘energy intensity in health systems’ , ‘peak fat’ , ‘5% health in Cuba’, ‘the Quantified Self’ , ‘Design grammars for health and care’ , ‘doing what we know we need to do’. It builds on the chapter on Conviviality in my book In the Bubble].
My core proposition at the Mayo event was that peak oil, and peak fat, are transforming the logic that currently shapes the global biomedical system. Firstly, because coming energy famines will render one of the world’s most energy-intensive systems unsustainable. And second, because until the medical system addresses the causes of illness with the same brilliance with which it addresses the effects, the population will continue to get sicker.
Energy intensity
The main Mayo Clinic building is a vast silver facility that shouts two things: authority, and energy intensity.

If one Googles health, and energy efficiency, most results are about hospital buildings and attempts to render them ‘greener’. But hospital buildings are just one element within a distributed system that is both materially heavy and entropically complex.
For a start, most of the consumables within any hospital are oil-based – from analgesics and antihistamines, through heart valves, implants, and prosthetics, to ambulances and helicopters.
But energy that you can measure, such as that used by buildings and suppositories – is only one part of the picture.
A new technique called Systems Energy Assessment measures the total energy demand of businesses, such as health ones. Its developers have concluded that for every barrel of oil equivalent that’s counted today – if they are counted at all – four times that number are consumed invisibly. And because they are neither perceived nor counted, no thought is given to their possible replacement.
A recent UK study, for example, found that five per cent of all vehicle movements on British roads are health-related.
There is some discussion in the medical world about the consequences of the coming energy crunch but by all accounts these voices find it hard to be heard and finds it an uphill struggle to make an impact.
Loud alarms raised in other other complex organisations are being taken more seriously. Lloyds of London, for example, an epicentre of the global financial system, warned last year in a report called
Sustainable Energy Security that “an oil supply crunch is likely in the short-to-medium term”.
And the US Army, hardly a hotbed of doomers and subversives, stated in its Joint Operating Environment [JOE] report that “by 2012, surplus oil production capacity could entirely disappear…we simply aren’t going to replace this with renewables”.
The danger facing complex organisations such as the Mayo Clinic is that, by postponing consideration of energy issues, it risks catabolic collapse down the line. This is the situation, as described by John Michael Greer,in which by the time a system realises that its energy regime is not sustainable, the money energy and resources to do anything about it are no longer available.
Peak fat
From catabolic collapse I moved on in my talk to peak fat.

We heard several case studies about innovative ways to deal with consequences of the diabetes pandemic – a disease growing in the US by a terrifying 30% a year. The response of designers and doctors was an array of Personal Health Planning tools, “high-end wellness” services, superfoods, remote diagnostics, and more. But almost nothing was proposed, that I heard, about tackling the causes of this grim disease on a mass scale.
Looking online I then found this statement by the Centers for Disease Control [CDC]. The mission of this Federal organisation is “to create the expertise, information, and tools that people and communities need to protect their health”.
On the subject of overweight and obesity, CDC’s website explains that these killer conditions “result from an energy imbalance. Behavior and environment play a large role… these are the greatest areas for prevention and treatment actions”
This is surely a bizarre statement. “The environment” makes you fat? I was under the impression that fat makes you fat – and the correlation between the growth of fats in the food system, and the growth of obesity and diabetes in the population, is not hard to spot. Neither is it a secret that the producers and distributors of this killer fat are the junk food and soft drinks industries.
The medical system – from the CDC to the Transform conference – appears to be focused overwhelmingly on downstream phenomena. Medical researchers are working tirelessly to improve treatment protocols – the steps for treating particular ailments. Huge efforts are also being made to improve safety in hospitals , and to raise the quality of care you receive in them.
But among all these projects, attempts to transform a food system, that is making hundreds of millions of people sick, are rare to invisible.
A speaker from Pepsico added to the cognitive dissonance.
Dr Dondeena Bradley told the conference that she is “on a journey… to redefine what nutrition means” and that her employer is determined to “double its food-end healthier portfolio”. I wanted to ask, “healthier than what?” – but was then distracted by her assertion that “we don’t have enough land in the US for everyone to eat their five a day”. I believe she probably meant to state “food system” rather than “land”; if not, she urgently needs a better map.
Even then, one has to ask if this is not a dead-end road. The only way for Pepsico to make money in the food industry is by processing food, and it is surely self-evident by now that processing, a.k.a. innovation – is bad for food.
Over one third of the added sugars that Americans consume are from sweetened carbonated beverages such as Pepsi. Healthy food – fresh- from-the-field food, whole-until-the-kitchen food – loses quality with each ‘value-adding’ innovation process it is subjected to.
A more plausible proposal from a global business was made by IBM’s Dr Paul Grundy. The conference responded enthusiastically to his Patient Centered Medical Home.
Grundy is one of the world’s leading experts on preventive medicine, so he did not come to peddle platitudes. His model integrates phone, e-mail and Web portals to enable one-on-one communication and collaboration between doctors and patients. Each occupant of the Home will enjoy an ongoing relationship with a doctor for continuous and comprehensive care and – the killer line – “we know that somebody who has a personal physician will cost us about a third less”.
But a third less than what? The IBM scenario is enticing, but it suffers from two flaws. The first is cost. “A third less” will be welcome to those fortunate people who are employed, or in work, and are therefore insured. But it is likely to be unaffordable for the majority of the US population who need it most. Of course if IBM’s share of the pie, and that of highly-paid doctors, were to be removed from the equation, the story would probably be different. But as it stands, the PCMH is for the top 5%, not the bottom 95%.
The bigger drawback, from me, is that the PCMH is about one-to-one conectedness through technology. The secret to health transformation surely lies in the social, embodied, eye-to-eye, breathing-the-same-air kind of connectivity that sustains healthy communities elsewhere in the world.
5% health already exists
In Cuba, for example, where food, petrol and oil all have been scarce for 50 years as a consequence of economic blockades, its citizens “achieve the same level of health for only 5% of the health care expenditure of Americans.” (SCIENCE, 30 April 2010)
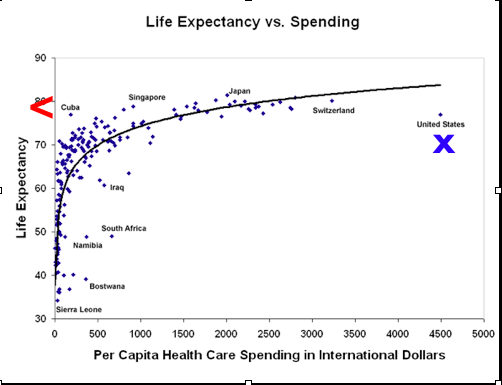
The reasons for this achievement are not magical. A key principle of the Cuban system is that physicians are based in neighbourhoods, not in clinics or hospitals. An estimated 97 per cent of medical care in Cuba is from neighbourhood-based family doctors and community health practitioners. Cuba has one family doctor per 180 inhabitants compared to one per 480 in the US.
Over in New Mexico, Community Health Workers in Project Echo are paid $10 an hour for their work in a highly effective campaign against common diseases such as hepatitis, asthma, and substance misuse.
In some of the state’s prisons, inmates, after a ten week training course, are proving highly effective health educators to their peers – and they are paid, if I understood the presentation correctly, nothing.
“Doctors”, said one development professional at the conference, when describing a project in Africa, “are grossly overemphasised”. This speaker told us how maternal deaths of women during childbirth had been reduced by a third following a training programme for traditional birth attendants. Experts, including doctors, had helped to set the training programme up, but most of the direct contact was among the same women as before.
Does one need to live in an impoverished or boycotted state in order to achieve 5% health?
No. In Northern countries, too, 5% health care already exists – but for the most part invisibly, or at least uncounted. This is is because value is the so-called social economy is created by caring relationships between people, not by the provision of care by a supplier. Indeed seen through this lens, the vast majority of care takes place away from medical establishments or the presence of professionals.
An example that I gave at the conference concerns dementia care and the Alzheimer 100 project carried out as part of the UK Design Council’s social innovation biennial Dott07.
700,000 British citizens suffer from dementia, and 3,000,000 people directly affected as family members and/or carers – and these numbers are expected to double every twenty years. How, people have started to ask, will the government care for them?
The answer is that it won’t. It can’t. Or at least, it cannot if the words ‘care for’ are interpreted to mean the complex, high-cost, energy-intensive and institutionally-focused kinds of medical care that are already bankrupting advanced countries.
In Dott07, confronted by this realisation, we reframed the words ‘care for’ and asked, instead: “What practical actions would improve daily life for people with dementia and their carers?”.
With that as our reference, we then worked over a two year period with a wide variety of citizens: people with dementia, carers, support and voluntary groups, researchers, doctors, nurses. We used a variety of approaches to determine what the needed practical actions might be at different stages of what we called ‘patient journeys’.
From this process emerged a wide variety of anecdotal insights and also, crucially, a shared understanding of what, for people with dementia and their carers, were priorities.
The two most pressing priorities for them were first, the awful experiences people have when they first discover they have a problem; and second, end of life experiences. These two issues were both more than twice as important as, for example, assistive technology, or communication campaigns to reduce stigma associated with the condition.
These insights, and understanding of priorities, enabled our project partners to identify a shortlist of service innovation opportunities: a care concierge; a buddy system; and an e-bay for time. The Dott project selected the development of a prototype dementia signposting service to enhance connectivity among existing support ecology. [Since then,this service has been adopted and developed nationally by the UK Alzheimers Society. And the Design Council has launched a new project called Living With Dementia.
The lesson from Cuba, New Mexico, and for that matter from the UK, is that as well as addressing causes rather than effects, community-based health and care is so massively cheaper than its mainstream alternative, and more effective in terms of overall health, that the time has surely come to regard the bottom of the pyramid as the top when it comes to healthcare innovation.
5% health by numbers
5% health is not about a u-turn back to a pre-scientific age. It’s about reconfiguring the way patients, doctors and researchers relate to each other.
Transformation looks impossibly hard from inside today’s official health systems. The prospect of radical change looks more doable outside the tent. Agile, networked knowledge-sharing thrives in the open open source movement, for example, whose vitality is sustained not by money, but by a shared sense of values.
One can also look outside the tent in time, as well as place. Open source has much in common with medieval kinship communities . These too were sustained by a duty of care among extended networks of family relationship and reciprocal obligation.
The trick is to combine ancient cultural values with new tools. As an example: The mass polling of patients to determine what actually works among new – and old – approaches.
Health geeks at the Mayo conference were confident that “patient-driven hypothesis generation” and “innovation through data liquidity” can achieve quickly what it now takes the academic publishing process years to achieve: put a possible solution out there; then find out from real people if, and how well, it works.
An organisation called Lybba http://www.lybba.org/work/, for example, is developing the platform for a a Collaborative Chronic Care network [C3N] [see also pic].
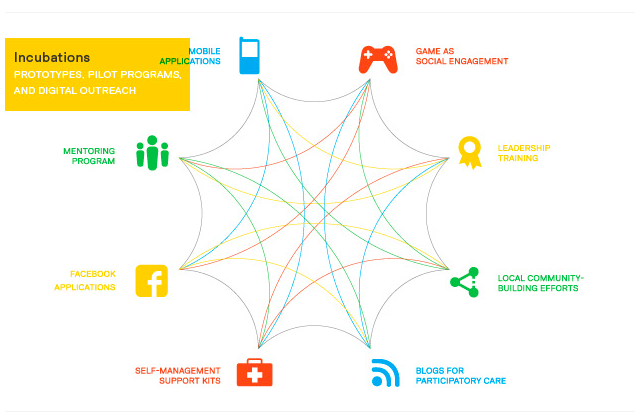
C3N will combine social- and idea-networking functions, “remote wellness tools”, and medical content.
A website such as CureTogether, for example, is already able to ask 6,000 patients, who suffer from anxiety, what treatments work best for each of them. The aggregated results are fascinating: totally free remedies, such as “exercise” or “masturbation”, are plotted on the same effectiveness versus cost chart along with commercial drug therapies. The anxious person gets to choose.
Information designer Hugh Dubberly and computer scientist Ian Eslick envisage a time when polling data will be combined with data visualisation and some kind of Facebook of health to help people make better choices about their health and behaviour.
The idea of self-made health data seems to have struck a chord. Among the Quantified Self crowd, for example, ‘self-tracking’ is growing fast; they use smart-phone apps and assorted custom-built devices to monitor patterns of food intake, sleep, fatigue, mood, and heart rate.
Me meters – or we meters?
I confess to a slight prejudice against the word “self” here.
We-meters, more than me-meters. would help us focus on the community more than the individual. Groups are a better compost for the growth of health alternatives. Too much emphasis on individual behaviour – for example, to eat less bad food – diverts attention to structural factors, beyond the individual’s control – such as food deserts.
I may well be mis-representing self-trackers here; they talk as much about the aggregation of data, as about its collection. Besides, an exciting prospect is that crowd-sourcing will be used to create a wide range of resources for alternative health care networks as three basis of a radically decentralised health ecology. A
llan Chochinov told us about the Open Prosthetics Project that is already producing useful innovations.
Before energy famines begin to impact seriously, we need to finds new ways to produce and distribute the essentials of modern medicine, such as vaccines and antibiotics. There could be mass calls for proposals for ultra low-cost therapies, services, or devices; groups would bid online to meet that need.
Design grammars for health and care
When we started work on Alzheimer100, we anticipated that the project would deliver a set of design methods and tools. These, we hoped, could be used to improve the experience of patients within the existing health system.
In the event what emerged – for this writer at least – was a realisation that the transition to a 5% health system is less about tools and more about new ways of perceiving the situation.
The late David Fielding, in his extraordinary book Lean Logic, calls these new ways of seeing ‘grammars’. [page 379]. In that spirit, here follows a first attempt to describe some grammars for the transformation of health care:
a Shift the focus of attention upstream. Health and wellbeing are properties of a social and ecological context in which soil, plant, animal, and man are interconnected in diverse communities and situations. That context needs to be cared for and, if necessary, repaired.
b Health and wellbeing are not something you ‘deliver’, like a pizza. This is no small shift of emphasis. The ‘delivery’ metaphor is pervasive in today’s system – as is the word ‘industry’. But those words perpetuate the myth that health is something produced by one set of people [the professionals] for another [their customers].
c Focus on the existing metabolic energy of people – not on the about-to-be-problematic fossil-fuel energy n mainstream medical systems. The good news is that 95% of care happens outside the medical system already; think of those three million Brits people caring for people with dementia today. The raw materials for transformation are already in place.
d Time intensity is bad for bottom lines – but great for ecosystems. [Remember those dementia patients and their carers in Britain? They judged trust between people, built up by co-presence over time, to be twice as important as the ‘delivery’ of services by third party vendors].
e Stop talking about ‘intervening’ in communities.Think of this way: you don’t intervene in a garden, you look after it. Care is more about breathing the same air than delivering the right solutions from afar.
f The same goes for ‘making an impact’. By what right do any of us presume to impact on someone else’s situation? It sounds like a meteor. 5% health is more about being in an ecosystem, and enhancing existing social energy – than about having an impact on it from above. This is one of the secrets to Cuba’s public health success. It has a lot of doctors [one for every 174 citizens, compared to one for every 600 in the UK] – but rather few of them hang out in clinics, or hospitals. Nearly all of them are based in a community.
Doing what we know we need to do
The many designers present at the conference were thrilled, and rightly, that the Mayo Clinic has established a Centre for Innovation that has design thinking at its core. But there’s a danger, amidst the euphoria, that priorities will get skewed.
Yes, good design can improve a patient’s experience. Yes, there are many ways that interacting with a doctor, being in a medical facility, or communicating with a service remotely, can be improved. And yes, of course, there’s good business to be done in the medical ‘space’.
But given the imminence of post peak energy famine; given what we now know about the causes of ill health, such as peak fat; and given that 5% models already exist for effective health: are high-end medical systems really the best place to focus design’s creative capacity?
Towards the end of the conference Rebecca Onie asked the key question: “why don’t we do what we know we need to do?” in health care.
She’s right. Most of the pieces for a profound transformation of the healthcare jigsaw are on the table. What’s missing is an evocative source image with which to direct everyone’s efforts where the greatest difference can be made. Could this be where designers can make a difference?
The challenge is not a shortage of ideas – crowd-sourced or otherwise. The challenge is a misallocation of resources.
Out there in the world, we know what will make a huge difference: localised food systems, clean drinking water, training and resources for community health workers on the ground. Essential, life-saving interventions such as childhood immunization, safe pregnancy and delivery services for mothers, access to treatment for HIV/AIDS, malaria and tuberculosis.
This is not to suggest that designers retrain as community health workers en masse. But one thing we could attend to, and now, is that missing source image for the 5% health jigsaw – the one in which communities are at the centre, in their own contexts, and health care experts and support services are located around the edge in a supporting role.
Mayo Clinic has the values to embrace this new picture and make it its own. It is also strong enough to begin growing a sequel system now, rather than waiting until the current one stops working.
In the Center for Innovation, the Mayo already has a stepping stone to the solidarity economy in place. I can can absolutely imagine that the Mayo community, given a moment to reflect on what lies ahead, could move to a strategy of what the ecologist David Fleming in Lean Logic describes as “deconcentration” – a radical refocus of the clinical context away from hubs and towards local expertise and self-reliance in context.