In 2011 I gave a talk at the famed Mayo Clinic. My suggestions were:
a Shift the focus of attention upstream. Health and wellbeing are properties of a social and ecological context in which soil, plant, animal, and man are interconnected in diverse communities and situations. That context needs to be cared for and, if necessary, repaired
b Health and wellbeing are not something you ‘deliver’, like a pizza. This is no small shift of emphasis. The ‘delivery’ metaphor is pervasive in today’s system – as is the word ‘industry’. But those words perpetuate the myth that health is something produced by one set of people [the professionals] for another [their customers].
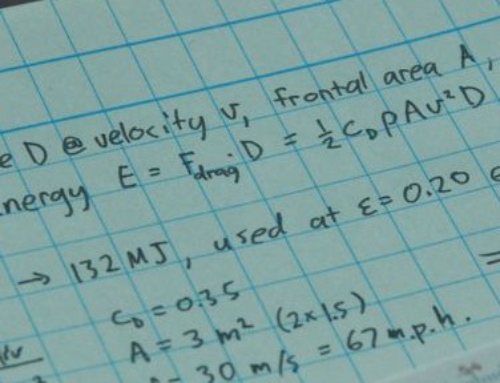
c The beauty of the health-as-ecosystem idea is that it enables us to focus on the existing metabolic energy of people – not on the about-to-be-problematic fossil-fuel energy on which mainstream medical systems depend. The good news is that 95% of care happens outside the medical system already; think of those three million Brits people caring for people with dementia today. The raw materials for transformation are already in place.
d Time intensity is bad for bottom lines – but great for ecosystems. We learned from working with dementia patients and their carers in Britain that they judged trust between people, built up by co-presence over time, to be twice as important as the ‘delivery’ of services by third party vendors.
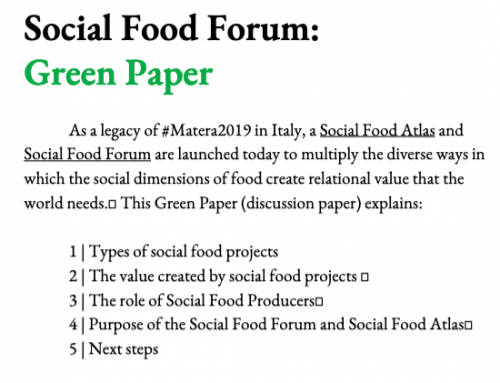
e When health is re-imagined as an ecosystem that needs to be looked after, it makes no sense to talk about ‘intervening’ in communities. Think of this way: you don’t ‘intervene’ in a garden, you look after it. Care is more about breathing the same air than delivering the right solutions from afar.
f. The same goes for making an ‘impact’. By what right do any of us impact on someone else’s situation? It sounds like a meteor. 5% health is more about being in an ecosystem, and enhancing existing social energy – than about ‘having an impact’. This is one of the secrets to Cuba’s public health success. It has a lot of doctors [one for every 174 citizens, compared to one for every 600 in the UK] – but rather few of them hang out in clinics, or hospitals. Nearly all of them are based in a community.
[These suggestions complement the chapter on Conviviality in my book In the Bubble].